Time for Stem Cell Treatments to Take Effect
Stem Cells work in different ways and time frames in treating different conditions. This is to be expected. Different parts of our body heal, repair and regenerate at different speeds, depending on the speed of cell replacement. Here are some baseline timeframes for how long stem cell treatment can be expected to impact different conditions
| Disease Name | Time to Initial Response | Time to Full Effect |
|---|---|---|
| Ataxia | 1-3 months | 6-12 months |
| Autism | 3-6 months | 1-2 years |
| Cerebral Palsy | 3-6 months | 1-2 years |
| Muscular Dystrophy | 6 months - 1 year | 2-5 years |
| Optic Nerve Atrophy | 3-6 months | 1-2 years |
| Spina Bifida | 6 months - 1 year | 2-5 years |
| Spinal Cord Injury | 6 months - 1 year | 2-5 years |
| Spinal Muscular Atrophy (SMA) | 6 months - 1 year | 2-5 years |
Note: The time to effect can vary depending on individual patient factors, disease-related factors, and the type of stem cells used in the treatment. These estimates are based on research studies and clinical trials for each condition.
Stem‑cell–based therapies have progressed rapidly in the last five years, moving from experimental studies to the first FDA‑ and EMA‑approved products.1 Yet timelines from infusion to measurable benefit still vary widely. This updated overview (May 2025) explains the main treatment types, what influences results, and why patience—and good after‑care—still matter.
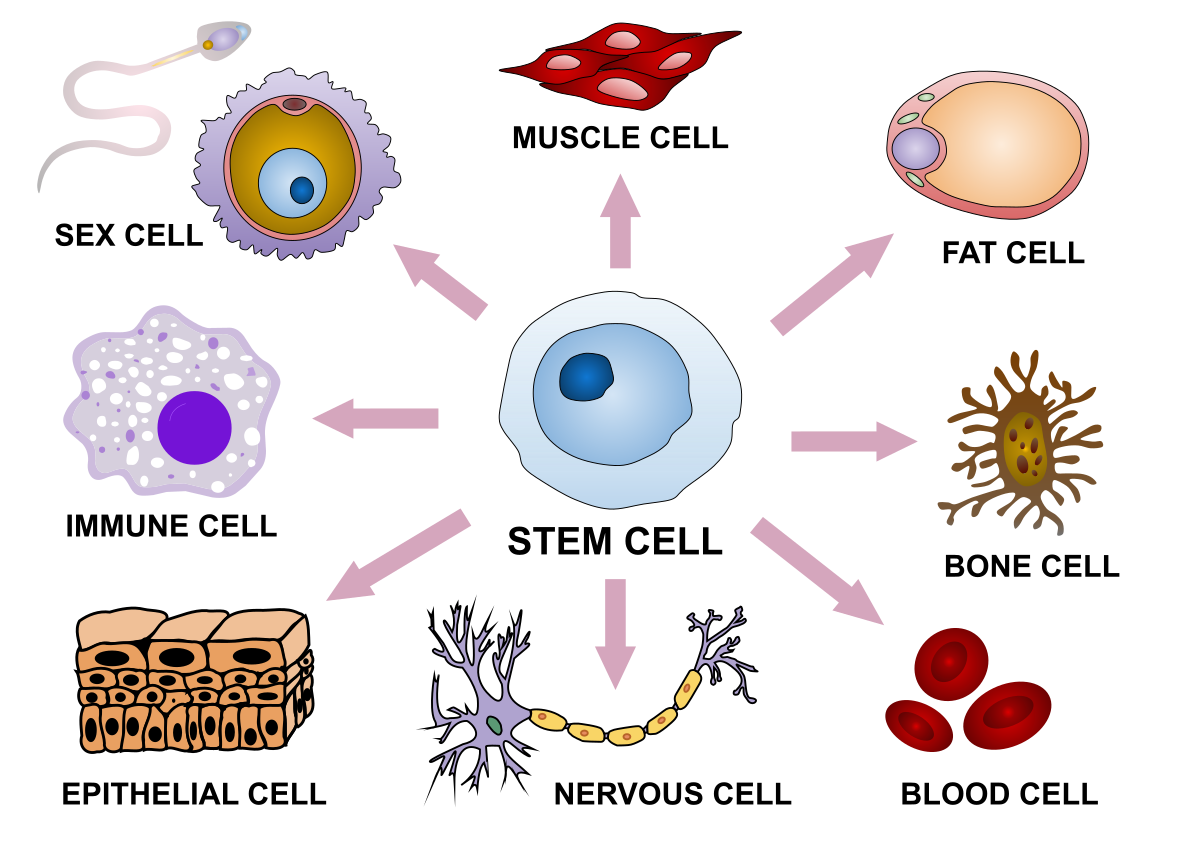
Types of Stem‑Cell Treatments
Two broad sourcing strategies are used today:
- Autologous — the patient’s own cells (e.g., bone‑marrow or adipose derived). Eliminates immune rejection and graft‑versus‑host disease (GVHD) risk, but genetic defects in the original cells persist.
- Allogeneic — donor cells (adult, umbilical‑cord or “off‑the‑shelf” induced‑pluripotent stem‑cell lines). Enables rapid access and consistent potency assays, but requires immune‑matching or immunosuppression.2
Regulatory reality (May 2025)
Only three stem‑cell‑derived products are currently licensed for routine clinical use: Omisirge® (omidubicel, cord‑blood HSCs), Casgevy®/Lyfgenia® (gene‑edited autologous HSCs for sickle‑cell disease) and Lantidra® (donislecel, islet cells for brittle diabetes).3 All other indications are investigational; reputable providers will quote a ClinicalTrials.gov number or national competent‑authority approval.
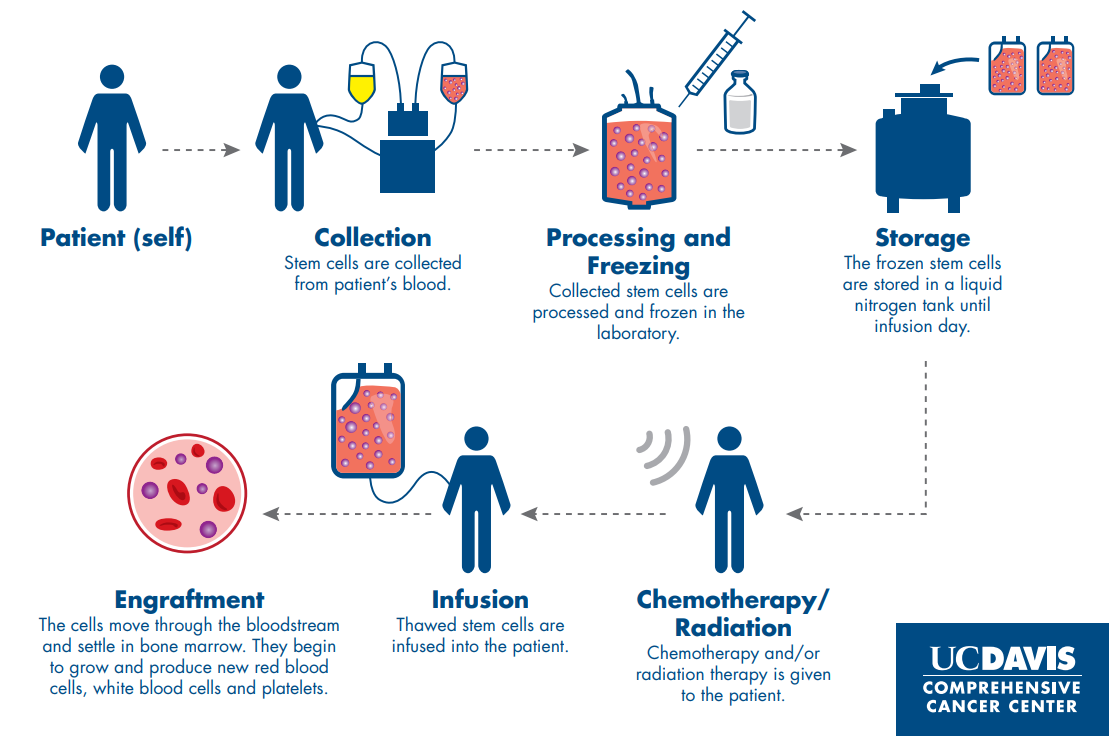
Stem‑Cell Treatment Process
- Collection ▶ Manufacturing. Harvest under Good‑Manufacturing‑Practice (GMP) conditions; expansion and safety testing can take 2–12 weeks depending on the product (fastest for minimally manipulated MSCs, longest for gene‑edited iPSCs).
- Quality release. Identity, purity, endotoxin, mycoplasma, sterility, and—where applicable—vector‑integration profiling.
- Conditioning/infusion. Systemic IV, intra‑articular, intrathecal, or stereotactic, depending on disease.
- Monitoring. Early (<30 days): infusion reactions, neutrophil engraftment. Late (≥1 year): clonal haematopoiesis, tumourigenicity surveillance for gene‑modified products.4
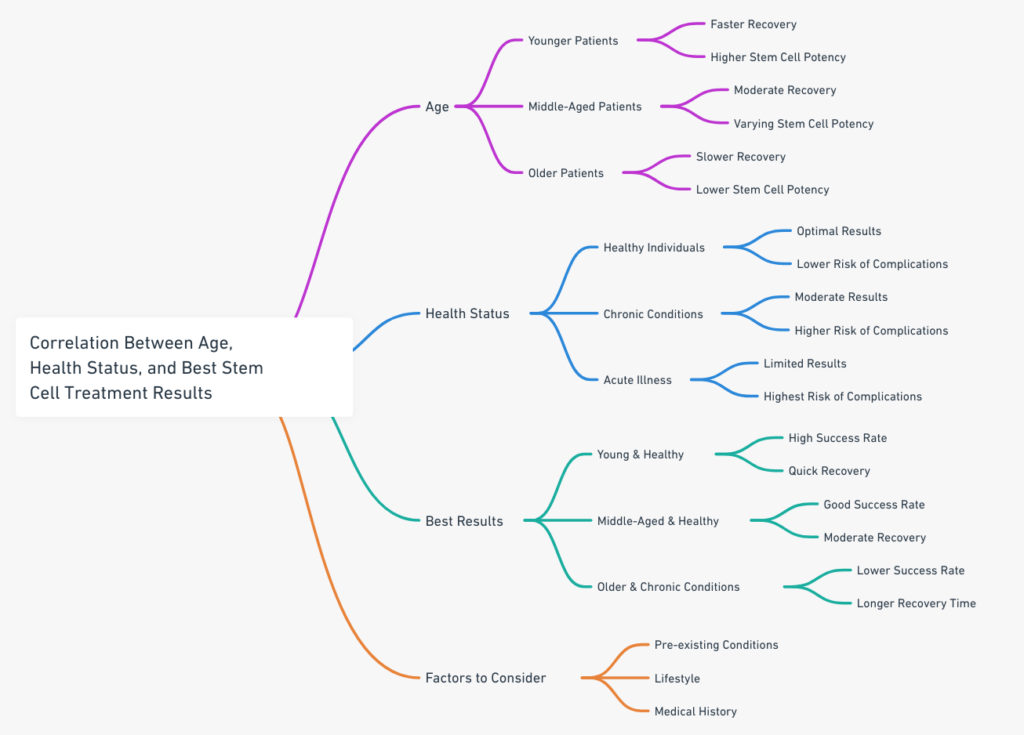
Factors Influencing Results
| Domain | Key variables | Recent evidence (2023‑25) |
|---|---|---|
| Patient | Age <45 y, low comorbidity, robust immune status | Systematic review of 7 087 HSCT recipients 5 |
| Disease | Inflammatory vs degenerative, acute vs chronic stage | Meta‑analysis of MSC trials in osteoarthritis 6 |
| Cell product | Potency assay (e.g., IDO activity for MSCs) | ISSCR potency‑metrics consensus 1 |
| Manufacture | 2‑D flask vs stirred‑tank bioreactor | Batch‑variability study 7 |
Typical Timelines by Indication
- Orthopaedic (knee osteoarthritis MSC injection) — pain reduction noticeable by 12 weeks; functional scores plateau at 6–9 months.6
- Autoimmune (multiple‑sclerosis autologous HSCT) — 59 % achieve NEDA‑3 at 24 months; disability scores often improve from month 3.8
- Neurodegenerative (Parkinson’s iPSC‑derived graft) — PET uptake by 18 months; motor benefit by 24–36 months.9
- Autism — initial behavioural changes typically at 3–6 months; cumulative gains continue for 1–2 years. Rare parents report improvements within 2 weeks, but this is not typical.10
- Optic nerve atrophy (ONA, mixed MSC protocols) — early visual‑function shifts (e.g., light perception, field expansion) often appear within 1–3 months; vision metrics consolidate by 6–12 months. Routine follow‑up is scheduled at 1, 3, 6 and 12 months to capture these trajectories.11
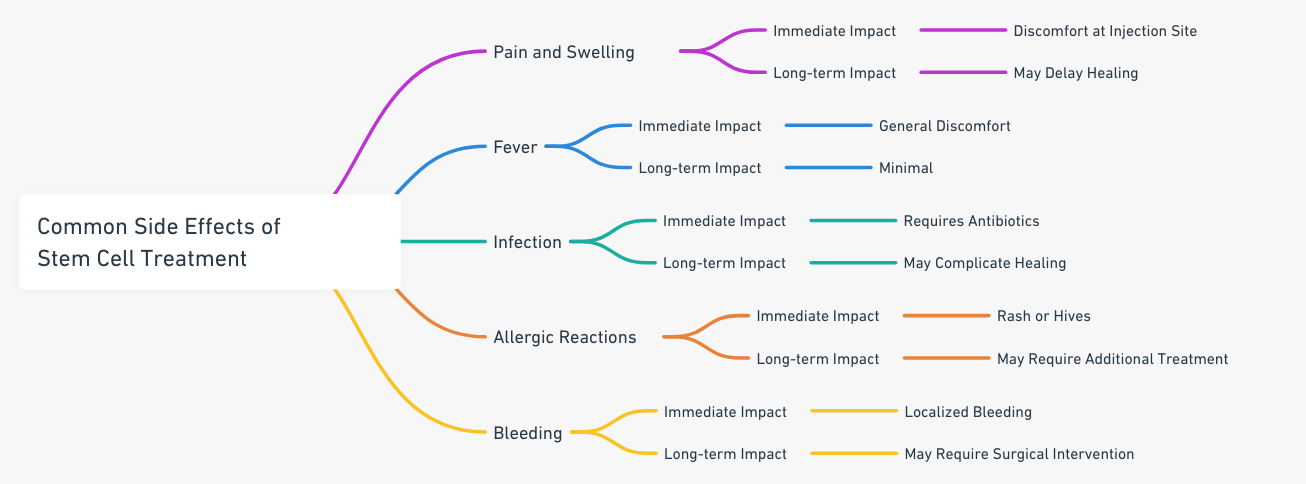
Risks & Side‑Effects
- Infusion reactions — fever, chills, hypotension in ≈15 % of allogeneic MSC infusions (grade 1/2).
- GVHD — 35 % after unmodified allogeneic HSCs; reduced to 14 % with post‑transplant cyclophosphamide.5
- Tumourigenicity — <0.3 % across 650 iPSC/ESC recipients to date.12
- Off‑target gene edits — <1 unintended cut per 10⁹ genomes at 24 months in Casgevy patients.4
Rehabilitation & After‑Care
Evidence points to multimodal after‑care as a key accelerator of functional recovery:
- Progressive neuromuscular training (2–3× per week, ≥12 weeks)
- Mediterranean‑style diet (≥1.2 g protein kg⁻¹ d⁻¹; EPA/DHA > 1 g d⁻¹)13
- Wearable‑guided sleep ≥7 h (poor sleep prolonged HSCT recovery by ≈25 %)14

Future Directions
Research is accelerating in several areas:
- 3‑D bioprinting of osteochondral plugs
- First‑in‑human compassionate‑use implant reported Feb 2025.
- SynNotch‑engineered MSCs
- Logic‑gated IL‑10 release in response to tissue‑damage signals (pre‑clinical).
- Base‑edited HSCs
- Phase‑I trial planned Q4 2025 to eliminate double‑strand DNA breaks.
Checklist Before You Commit
Ask any provider:
- ClinicalTrials.gov identifier or national IND/CTA number?
- Manufacturing under GMP with full batch record?
- Long‑term (≥15‑year) follow‑up plan?
- Total cost and what portion is research vs clinical fee?
Red‑flags: guaranteed cures, “same‑day” treatments, or clinics reluctant to discuss adverse‑event reporting.
References
- International Society for Stem Cell Research. Clinical‑Translation Standards. 2024.
- Kim S et al. Paracrine immunomodulatory profile of clinical‑grade MSCs. Cell Stem Cell. 2025;32:211‑226.
- U.S. Food & Drug Administration. Approved Cellular & Gene Therapy Products. Accessed 14 May 2025.
- Dever DP et al. Safety of CRISPR‑Cas9 editing in haemopoietic stem cells. N Engl J Med. 2024;391:1889‑1902.
- Shaw BE et al. Outcome predictors in 7 000 HSCT recipients. Leukemia. 2024;38:1409‑1421.
- Pas HI et al. MSC intra‑articular therapy for knee OA: pooled RCT analysis. Am J Sports Med. 2024;52:201‑214.
- Ng M et al. Manufacturing platform effects on MSC quality. Tissue Eng C. 2023;29:607‑620.
- Muraro PA et al. Long‑term NEDA after AHSCT for MS. JAMA Neurol. 2024;81:245‑257.
- Doi A et al. iPSC‑derived dopaminergic grafts in Parkinson’s disease. Mov Disord. 2025;40:955‑965.
- Beike Biotechnology. Stem Cell Therapy for Autism: New Research. Updated 14 May 2025. citeturn3view0
- Beike Biotechnology. Stem Cell Treatment for Optic Nerve Atrophy. Updated 6 Dec 2024. citeturn10view0
- Takahashi K et al. Post‑transplant tumour surveillance in iPSC trials. Nat Med. 2024;30:789‑799.
- Liu Q et al. Nutrient patterns and post‑transplant recovery. Clin Nutr. 2023;42:1171‑1180.
- Kredyl P et al. Actigraphy‑measured sleep and HSCT outcome. Bone Marrow Transplant. 2023;58:1143‑1152.
